The top five tech solutions that helped eradicate wild poliovirus in the African region
Ten years ago, health workers and volunteer vaccinators had to rely on hand-drawn maps and memory in order to reach every child.
Today Africa’s polio eradication programme has been transformed by technology and innovation. New systems have also brought an unprecedented level of accountability to the programme, ensuring high standards and data-driven progress. These tools have played an essential role in accelerating progress toward polio eradication.
Here are five of the most important technological innovations born from the polio programme:
1. GIS Mapping – data management with mobile technology
Geographic information system (GIS) technology combines mobile devices and mapping software to capture, analyse and present data.
While GIS software has been used for over 20 years to analyse health data and produce maps, “no other programme has used GIS in the structured way that the polio programme has taken,” says Kebba Touray, GIS Manager for the Polio Eradication Programme at the WHO Regional Office for Africa (WHO AFRO).
First used by the polio programme in northern Nigeria after a surge of polio cases in 2012, GIS allowed polio teams to use their mobile phones in order to target poorly covered areas and deliver polio vaccines.
These systems are not limited to polio eradication, however. When an outbreak of Ebola began in August 2018 in the Democratic Republic of the Congo (DRC), just a few hundred kilometers from Uganda, GIS surveillance data established for polio showed the location of cases along with population movement patterns. This enabled health officials to accurately target the 24 health zones along the 800 kilometre border that were most at risk. Uganda, as a result, managed to avoid a large-scale Ebola outbreak.

A polio surveillance officer downloads data from vaccinators' phones at the end of the day's polio vaccination campaign in Jere, Nigeria, 2020. ©️ Andrew Esiebo/WHO
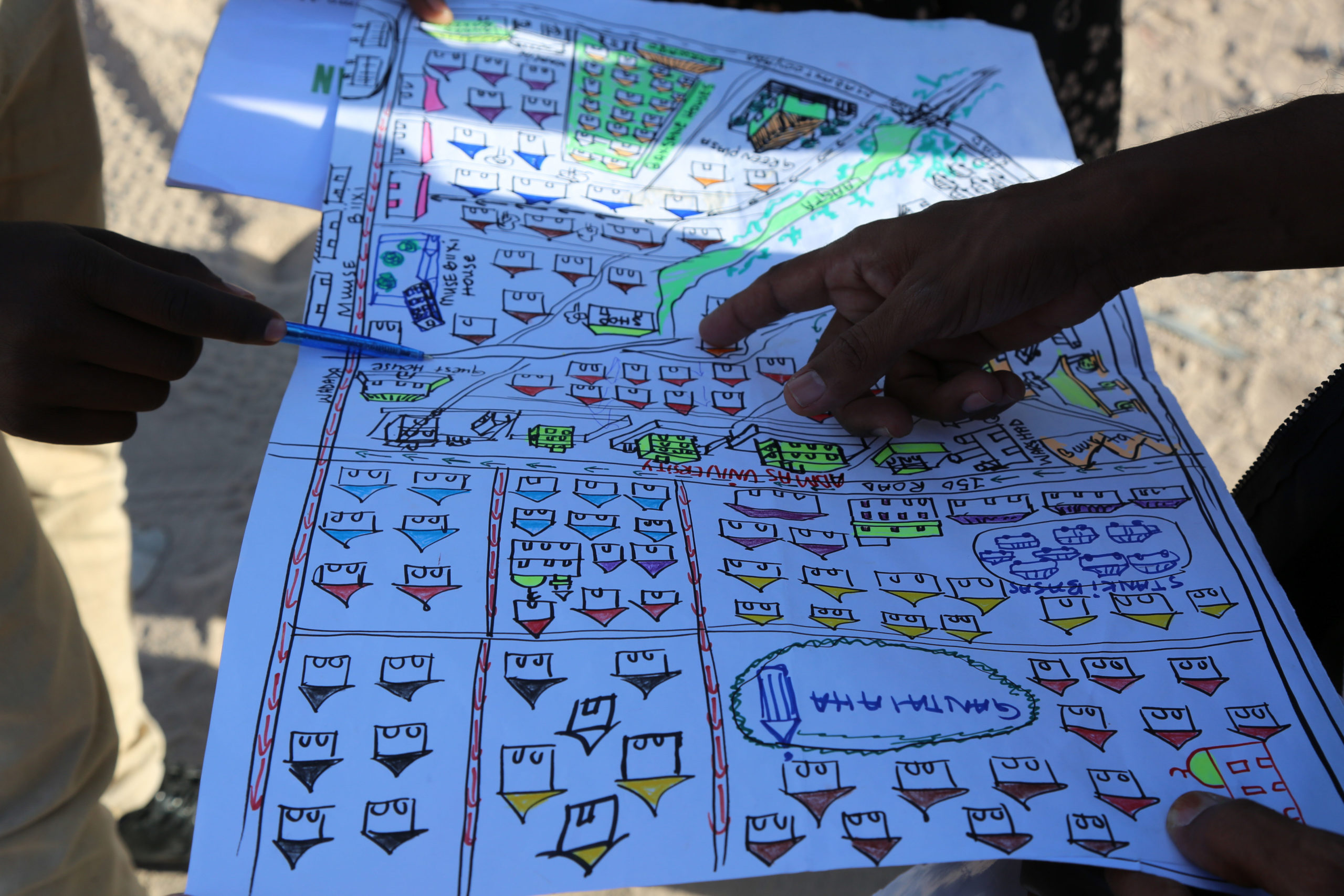
GIS applications are used alongside traditional maps, such as this one showing residential areas targeted for polio vaccination, Hargeisa, Nigeria, 2019. ©️ WHO
2. AVADAR – Auto Visual AFP Detection and Reporting
Formal healthcare is sparse in some parts of Africa where there is insecurity or weak health systems with limited reach. In these areas, some 10,000 trained community members have been trained to use Auto-Visual AFP Detection and Reporting (AVADAR). The network spans across ten countries in the African region. From traditional healers to village leaders, these community members report cases of polio-like symptoms to the ministries of health and WHO using an SMS-based technology on their mobile phones. The application was first piloted in 2016 in Nigeria, where insecurity had created blind spots in polio surveillance. Funding from the Bill & Melinda Gates Foundation then allowed AVADAR to be scaled up to other parts of the country.
Today AVADAR has also been used to find and report cases of Lassa fever, cerebrospinal meningitis and yellow fever, among others.
During the COVID-19 pandemic, the technology and vast AVADAR community network has proved invaluable. WHO stays in regular contact with community members, sending explanatory videos to help them spot and report potential COVID-19 cases, which means health officials across Africa are better able to detect potential outbreaks and target hot spots.
3. e-SURV – electronic surveillance for real time monitoring of field activities
Like maps, data collection for disease surveillance was once all done on paper. When reporting a suspected case of polio, health workers and community volunteers would fill out forms, which would pass through a number of hands before they, often days later, reached a health officer who could process the information and take action. Not only was this slow, but often involved significant duplication of efforts.
“There were many polio staff visiting health facilities asking the same things,” says Dr Ticha Muluh, Polio Surveillance Officer for the Polio Eradication Programme at WHO AFRO. “We needed a system that could monitor and visualize who went where in real-time, on a shared server.”
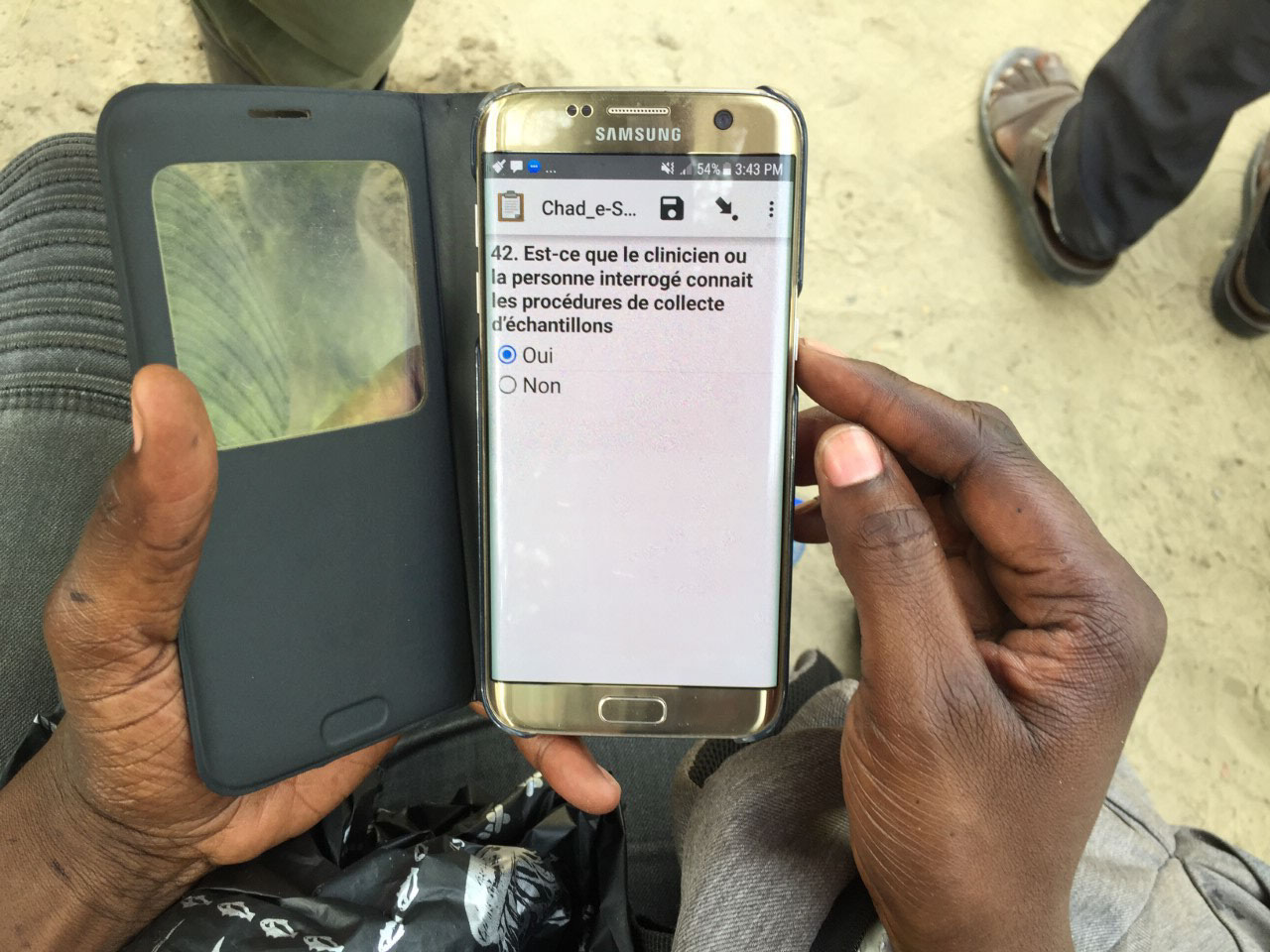
To address this challenge, polio surveillance officers in Maiduguri, Nigeria, developed a small checklist, which then became an electronic platform known as e-SURV. The tool comprises an electronic form accessed through a mobile application that also records staff movements for accountability. Rolled out in 44 African countries, e-SURV is now used beyond polio eradication to monitor routine immunization and identify disease outbreaks happening in an area.
4. Digital Elevation Modelling – improving environmental surveillance
While traditional poliovirus surveillance relies on finding and testing children with paralysis, testing wastewater and fecal material along sewage lines can serve as an early warning system for the presence of poliovirus. Environmental poliovirus surveillance was first used in Pakistan and Egypt, but is now used in 32 countries across the African region, with samples from 300 sites sent regularly for laboratory testing.
Although an effective method, environmental surveillance could still be ‘hit or miss’. In 2014, the addition of digital elevation modelling made it much more precise. It works by using three-dimensional maps that help teams adjust the location of sample collections to yield better results. The modelling also pinpoints with greater accuracy which areas might be affected if a sample tests positive for polioviruses.
Particularly helpful in isolating circulating vaccine-derived polio (cVDPV), digital elevation modelling has recently been used successfully in four cities in Angola, where there are repeated outbreaks, prompting vaccination teams to respond quickly. During an outbreak of cholera in South Sudan, the technology was also successfully used to identify the area in which children needed to be vaccinated, allowing the targeted rollout of oral cholera vaccines.
As wild poliovirus is eradicated and funding reduces, environmental surveillance – which is highly sensitive – will be a core tool in detecting cVDPVs.
5. eLQAS – electronic tracking of vaccination campaign quality
Since 2008, various quality assessments have been introduced to the African region’s polio programme. The most important of these are lot quality assurance sampling (LQAS) surveys, which measure the quality and approximate coverage of supplementary immunization activities and highlights where and why children are missed. As with other data collection, this used to be done by hand. Each stage the data passed through, there was also an additional risk of human error.
Electronic questionnaires avoid these shortfalls. Programmed onto smartphones, eLQAS is used to identify areas and households that are missed during immunization campaigns. In 2013, when eLQAS was used during supplementary vaccination campaigns in South Sudan, the results gave a much faster, more detailed analysis than previous paper-based LQAs. This information was then used to conduct mop-up campaigns and improve subsequent campaign quality.